Leigh syndrome (sometimes called Leigh’s disease) is a rare and severe neurometabolic disorder and a type of primary mitochondrial disease. Mitochondria extract energy from your food to help your cells do work. All of the cells in our body (except red blood cells) have mitochondria.
Judith, Israel

Never Forgotten, Ana, Romania
What are Mitochondria?
Mitochondria are the “powerhouses” of our cells, responsible for producing about 90% of the energy needed to sustain life. These tiny organelles are found in nearly all the cells of the body, except red blood cells, and play a crucial role in converting the food we eat and the oxygen we breathe into energy that powers cellular functions.
When mitochondria don’t work properly, it leads to mitochondrial diseases, where the body’s cells cannot generate enough energy to function effectively, often resulting in severe health issues.
What is Leigh syndrome?
Leigh syndrome, sometimes called Leigh’s disease, is a rare and severe neurometabolic disorder that falls under the category of primary mitochondrial diseases. Leigh Syndrome symptoms usually start between the ages of 3 months and 2 years. It can also occur in teenagers and adults, although this is less common.
Newborns with Leigh syndrome seem healthy at birth, and may reach major milestones on time. Yet the disease begins interfering with function of the central nervous system. That is why children with Leigh syndrome lose these abilities or experience other physical or developmental delays.

“Enjoy every day and celebrate the little things. See the world through your child's eyes - play in the rain, jump in the puddles, give them that extra cuddle at night - whatever they need because this disease is unforgiving and you never know when it may be the last kiss, cuddle, laugh or dance.”
- Kristi Lloyd, AustraliaMom to Lola who passed away from Leigh syndrome. Lola is missed by her parents, and 2 brothers.
What causes Leigh syndrome?
Our DNA is made up of DNA in the nucleus of our cells (nuclear DNA, half of which is inherited from the father and half of which is inherited from the mother, and mitochondrial DNA (which is in the mitochondria, inherited from the mother).
Leigh syndrome can be caused by nearly 100 nuclear DNA genes and 16 mitochondrial DNA genes, with more genes continuing to be discovered. Your doctor may order some genetic tests in blood (or a cheek swab, or a urine sample) in order to arrive at the exact genetic diagnosis.

Ben, Austria

Miller, USA
How many people does Leigh syndrome affect?
Leigh syndrome affects about 1 in 40,000 individuals. However, this number may be underestimated. Population variations, misdiagnosis, and even a reluctance by some medical professionals to use the term “Leigh syndrome” likely impact measurements of how many people actually have the disease.
What are the symptoms of Leigh syndrome?
Early signs and symptoms of Leigh syndrome are frequently not at all specific for the disease, as they may be caused by many other more common diseases. This means that it is often difficult to diagnose when the symptoms first start. These early problems may include:
- Lack of appropriate weight gain
- Poor feeding or sucking
- Diarrhea and vomiting
- Loss of motor skills or other developmental skills
- Lethargy and drowsiness
- Irritability or continuous crying
As the disease progresses, the symptoms typically become more apparent and may include:
- Neurological symptoms: Developmental delays, loss of skills, muscle weakness.
- Motor problems: Uncoordinated movements, muscle contractions, stiffness.
- Respiratory issues: Breathing difficulties, respiratory failure.
- Cardiac issues: Possible changes in heart structure (cardiomyopathy) or rhythm (arrhythmia).
- Cognitive and behavioral changes: Cognitive impairment, intellectual disability, mood changes.
- Optic atrophy: Vision loss or impaired visual acuity.
- Seizures: Generalized or focal seizures.
- Gastrointestinal issues: Poor appetite, swallowing difficulties, vomiting, diarrhea.
- Failure to thrive: Poor growth and weight gain.
It is important to keep in mind that while these symptoms and complications are possibilities, not everyone with Leigh syndrome will invariably develop each and all of these symptoms.
How is Leigh syndrome diagnosed?
Healthcare providers use multiple methods to diagnose Leigh syndrome:
MRIs and Imaging Scans
To look for damaged areas in the brain
Blood tests
To check lactic acid levels and other metabolic markers
Genetic tests
To identify the type of gene mutation causing Leigh syndrome and confirm diagnosis
Once confirmed, your doctor may monitor many different labs and organ systems and may refer you to other specialists for comprehensive care.
Is Leigh syndrome hereditary?
Leigh syndrome can be inherited or occur spontaneously.
There are several ways people inherit the gene mutations that cause the disease.
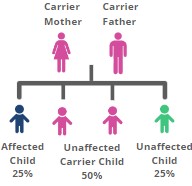
Autosomal recessive inheritance (most common)
In this type of inheritance, two dysfunctional copies of a gene are needed for a person to show the disorder. Each person has two copies of every gene, one from each parent. If both parents are carriers (i.e., have a single mutant copy) of the same mutant gene, they are unaffected. However, there is a 25% chance that their child will inherit two mutant copies of the gene (one from each parent) and show the disorder.
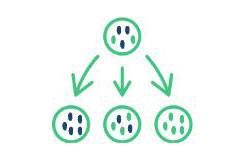
Maternal or mitochondrial inheritance (less common)
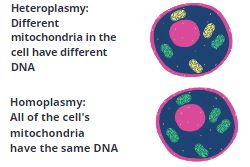
This type of inheritance is based on the genes that are found in the mitochondria. Unlike the rest of a person’s DNA, which is located in the nucleus of the cell and is inherited from both parents, mitochondrial DNA is inherited only from the mother. Disorders that are determined by the mitochondrial DNA may be passed down from the mother to all, some, or none of the children depending on the random amount of affected mitochondrial DNA that is passed down during reproduction.
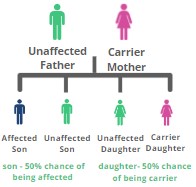
X-linked inheritance (least common)
In this type of inheritance, the gene responsible for the condition is located on the X chromosome. Females have two X chromosomes. Males have one X and one Y chromosome. As a result, it is often the case that males with X-linked conditions are more severely affected, as females have the other X to compensate (this is not always the case, and in some conditions males and females with X-linked conditions are similarly and equally affected). A male has a 50% chance of inheriting one mutant copy of the gene from his mother. When this happens, he will show the trait or condition. This is because he does not have another X chromosome with a normal copy of the gene to compensate. Females are less likely to manifest or have X-linked conditions. This is because they have a second X chromosome with a normal copy of the gene. However, females with X-linked genetic conditions may still show signs of it depending on the nature of the underlying condition.
The presence of multiple variants of mitochondrial DNA within an individual’s cells is known as heteroplasmy, while homoplasmy refers to a condition where all copies of mitochondrial DNA are identical.
Very rarely Leigh syndrome can be inherited in autosomal dominant pattern, with only one gene (DNM1L) known at this time. Autosomal dominant inheritance occurs when an individual inherits a single copy of the disease-causing gene from either parent.
Symptoms of Leigh Syndrome can also be caused by a de novo mutation, which is a type of mutation in either nuclear or mitochondrial DNA that occurs spontaneously in the affected individual and not inherited from either parent.
Nuclear DNA genes associated with Leigh syndrome
AARS2, ACAD9, ACO2, AFG3L2, AIFM1, APOPT1, ATP5A1, ATP5E, ATPAF2, AUH, BCS1L, BOLA3, C12orf65, COQ2, COQ4, COQ6, COQ7, COQ8A, COQ9, COX10, COX14, COX15, COX20, COX6B1, COX8A, CYC1, DARS2, DGUOK, DLAT, DLD, DNM1L, EARS2, ECHS1, ETFDH, ETHE1, FARS2, FASTKD2, FBXL4, FH, FOXRED1, GCDH, GFER, GFM1, GFM2, GTPBP3, GYG2, HMGCL, HTRA2, IARS2, IBA57, ISCA2, LARS2, LIAS, LIPT1, LRPPRC, LYRM7, MARS2, MFF, MFN2, MPC1, MPV17, MRPL44, MRPS22, MTFMT, MTPAP, NARS2, NDUFA1, NDUFA10, NDUFA11, NDUFA12, NDUFA2, NDUFA4, NDUFA9, NDUFAF1, NDUFAF2, NDUFAF3, NDUFAF4, NDUFAF5, NDUFAF6, NDUFAF7, NDUFB11, NDUFB3, NDUFS1, NDUFS2, NDUFS3, NDUFS4, NDUFS6, NDUFS7, NDUFS8, NDUFV1, NDUFV2, NFU1, NUBPL, PC, PCCA, PCCB, PDHA1, PDHB, PDHX, PDP1, PDSS1, PDSS2, PET100, PNPT1, POLG, RARS2, RMND1, RRM2B, SCO1, SCO2, SDHA, SDHAF1, SERAC1, SLC19A3, SLC22A5, SLC25A46, SUCLA2, SUCLG1, SURF1, TACO1, TARS2, TK2, TMEM70, TPK1, TRMU, TSFM, TTC19, TUFM, TWNK, TYMP, UQCC2, UQCC3, UQCRQ, VARS2
Mitochondrial DNA genes associated with Leigh syndrome
MT-TW, MT-TL1,MT-TL2, MT-ATP6, MT-CO3, MT-ND1, MT-ND5, MT-ND6,MT-TV, MT-TV, MT-TK, MT-ND2, MT-ND3, MT-ND4, MT-TI

Delta, USA
Is it possible to prevent passing on Leigh syndrome to your child?
Family planning options for Leigh syndrome depend on the type of inheritance. For more information please download the family planning guide below.
We thank the authors and contributors who helped with the development of this page: Kasey Woleben, Sophia Zilber, Courtney Boggs, Shamima Rahman, FRCP, FRCPCH, PhD, Ibrahim Elsharkawi, MD, Breanna Lima Martinez, MS, CGC, Melinda J. Burnworth, PharmD, BCPS, FASHP, FAzPA, Titilola M. Afolabi, PharmD, BCPPS, Peter McGuire, MD, Krisztina Ferencz, Rachel Kramer, PhD.